

This article is part of your HHCN+ membership
The offering of behavioral health services in the houses of patients can make the services more effective and better, but an already complex regulatory and reimbursement landscape for these services is expected to become even more difficult.
In view of the large Medicaid shortcuts taken into account in the Senate, the states will increasingly finish financing for home and community-related services at home and reimbursement of reimbursement for health care at home. The lawyers for the maintenance of home care are pushing for comprehensive regulatory reforms in order to protect access and keep the critical services pace with increasing demand.
“However, the health needs of the behavioral complaints escalate nationwide, especially in the case of medicaid and twice-legged population group and political framework conditions, have not remedied with the requirements for delivery at home in the home,” said Kristen Palumbo, Chief Operating Officer and Chief Compliance Officer at Innovive Health Care News.
Medford, innovive based in Massachusetts, offers patients with several medical comorbidities with behavioral disease diseases in-home health services. Innovive offers qualified nursing, which should support mental and physical health, wound care, behavioral medicine and nursing coordination, among other things.
Every year each of five Americans experiences a condition of behavior. Among the Medicare beneficiaries, the rate is even higher and affects one of four people.
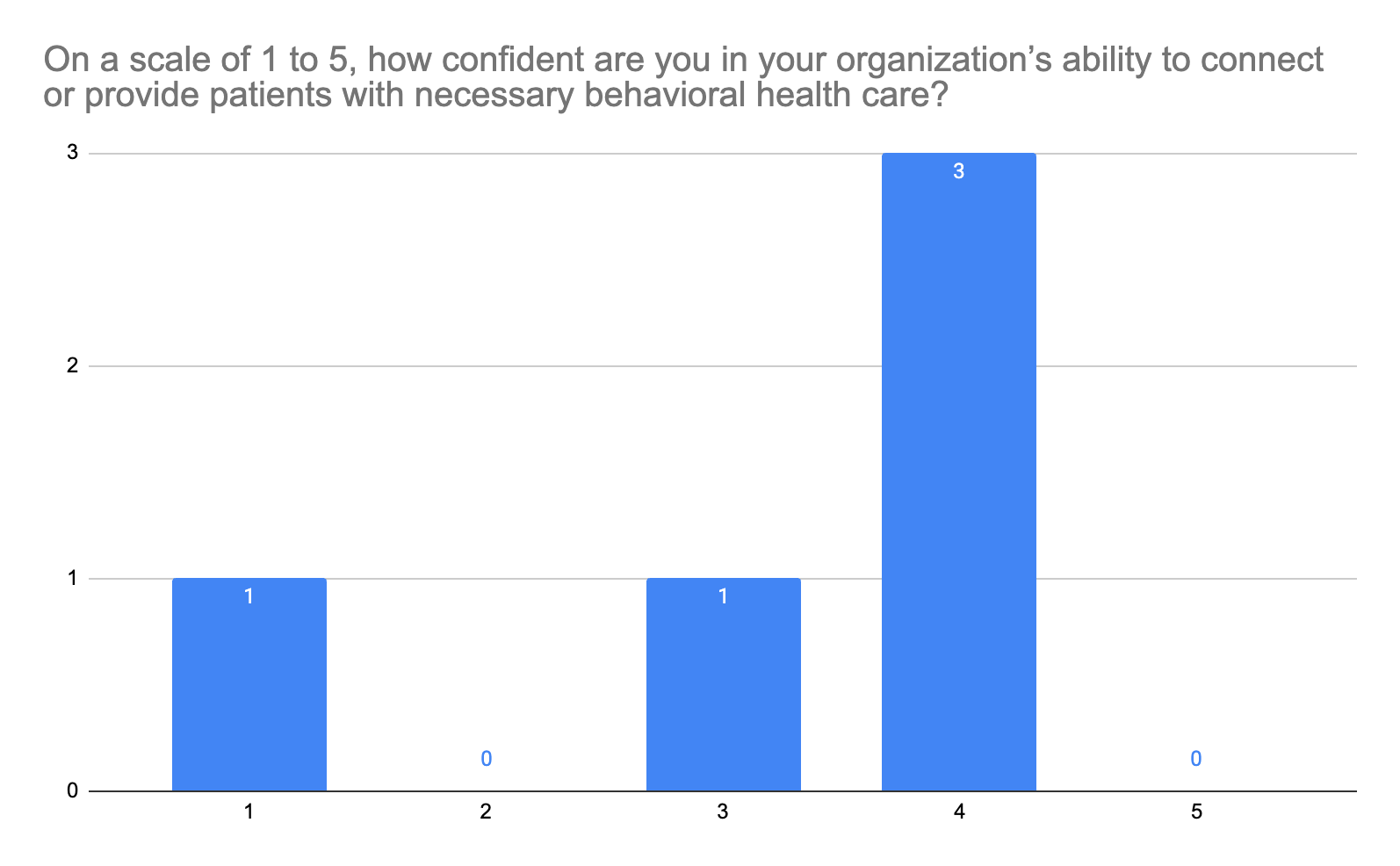
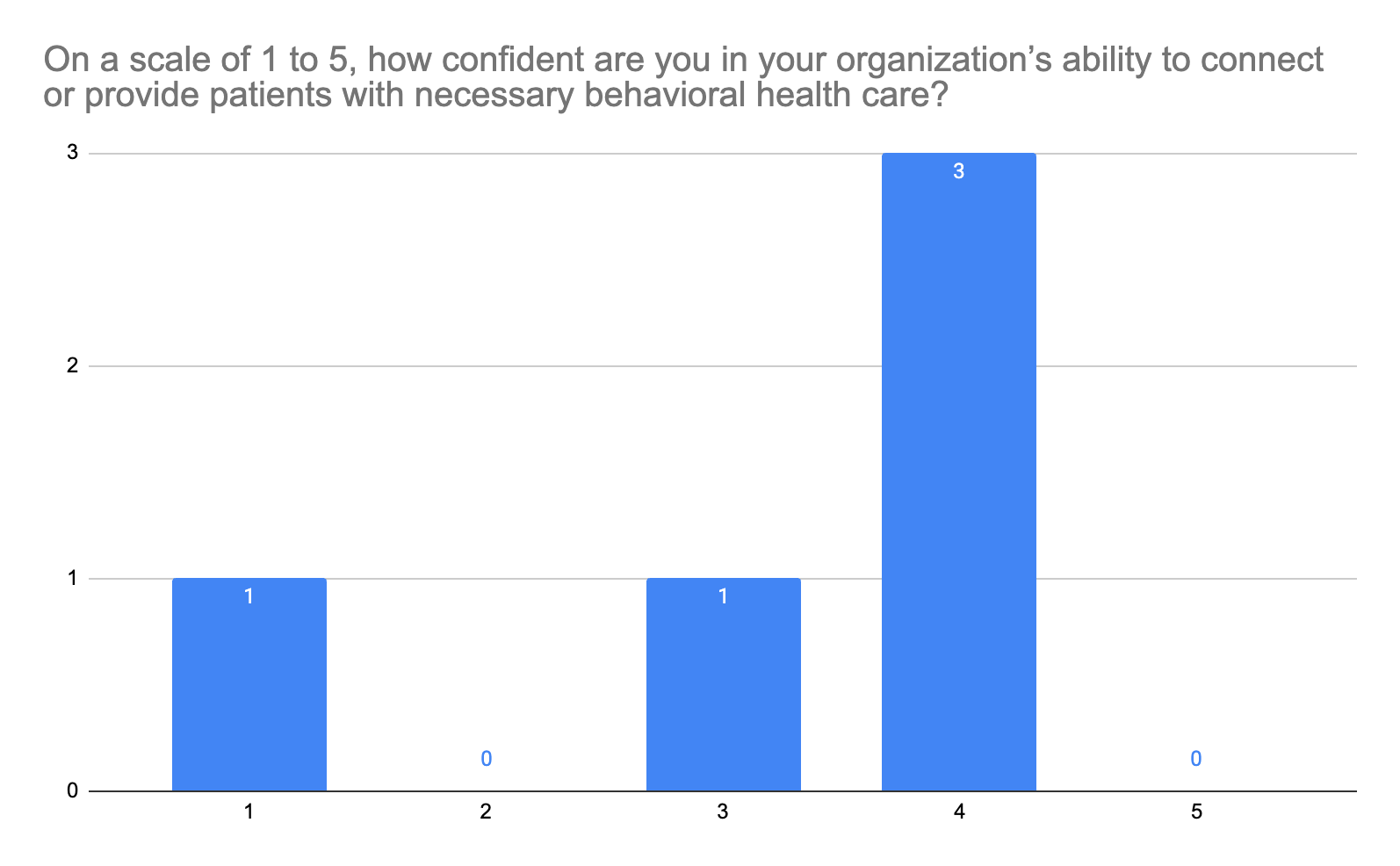
Despite the frequent concerns regarding behavioral health, even large organizations of the healthcare system for home health care may not be fully equipped in order to deal with the behavioral health needs of their patients. In a recently carried out HHCN survey, none of the five respondents stated that they could be 100% confident that their organization could connect or provide the patient with the necessary behavioral medicine.
According to Dallas Star, Regional Director of Behavioral Health at Bayada Home Health Care, over time over time, over time, has behaved over time. The availability of ABA services (applied behavioral analysis) has currently shifted in favor of in-clinic supply.
“While clinically-based care offers its own advantages, a multi-setting approach that is supported according to standards such as those of the Council of Autism Service providers (CAPP) is crucial to cover the various customer needs,” said Star. “Organizations like Bayada want to bridge these gaps by offering services in various environments, including houses, municipalities, schools and clinics, to ensure that the supply is delivered wherever the customer needs the most.”
Bayada in Pennsauken Township, New Jersey, is a non -profit provider of domestic health services that offers qualified and non -qualified home care services, child health, home care, rehabilitation and aid organization.
Shifts to in-clinic behavioral health care are limited access to the care of people with profound autism, which often need home care or care in residential areas.
The regulations and guidelines of domestic providers of behavioral health must follow
Organizations that offer behavioral medicine must comply with both the federal regulations and the country-specific guidelines that vary significantly from one state to another.
For example, Innovive is active in Massachusetts, Colorado and Iowa, and according to Palumbo, every state has a “different” regulatory environment. In order to maintain compliance, innovive maintains localized and centralized compliance and clinical teams in every state.
Some of the innovive regulations must comply with CMS participation conditions, state license rules, Medicaid regulations and data protection standards according to hipaa and 42 CFR part 2.
Some states have additional requirements for domestic settings, such as stars like an electronic visitor test (Eff).
“In the state Medicaid programs, there is a lack of consistency that difficult to operate for providers who serve several states,” said Star.
The regulations vary depending on the payers and state-by-state variations. The coverage of Medicaid for ABA Care is usually limited to people aged 21 and over, Star said, and Medicare currently does not cover ABA services and limits access to the care of them.
The future of behavioral health in the household
Medicaid's financing of domestic and community -based services for people with mental illnesses is, according to the health matters of Dennis Heaaphy, Researchers and Political Analysts at Disability Policy in Boston, and Ellen Breslin, an order from National Health Care appointed Health Care (HMA).
The financing of domestic and parish -related behavioral health services has remained due to the institutional prejudices, Heaaphy told HHCN.
“In institutional bias, states must enable the financing of institutionalization, be it a nursing home or another institution, but domestic and community -based services are optional, although it is cheaper,” said Heaaphy. “In most cases, the states still choose institutionalization because it is basically simple or simple.”
Only 23 countries have used 28 exemptions and authorities to finance house and community services for people with mental illnesses and serious emotional disorders, while three to four times as many countries used these waiver for other population groups.
The already underfunded in-home providers of behavioral medicine feel increasing pressure from a weak regulatory landscape.
“The proposed Medicaid budget cuts and the current secretary for health minister for autism treatment have expressed concerns among the providers,” said Star. “Budget cuts could be the ability to attract and keep qualified employees for ABA services that have already been stretched thinly.
According to the Heaeaea, potential medicaid budget cuts will not have an impact on institutional care, but the home services suffer.
“The challenge [that states are] At the moment under the new administration, the states are exposed to enormous cuts in their Medicaid budgets, ”said Heaaphy. We are concerned that this could diagnose disproportionately people with mental health due to discriminatory practices and a lack of understanding of the needs of the population or influence disruptive disorders or substance disorders.”
Lawyers' efforts to improve access
In order to ensure long -term access to urgently needed behavioral health at home, providers are committed to higher reimbursement rates and increased support for providers, all of which can be facilitated by the increased introduction of value -based reimbursement agreements.
Innovive supports guidelines that promote the development of the workforce of experts for behavioral medicine in parish -based roles, stimulate value -based models that take into account the needs and complexity of behavioral health and ensure parity for psychiatric and medical services.
“The political decision -makers have the opportunity to redesign the house as a therapeutic environment and a sustainable alternative to institutional care,” said Palumbo. “By recognizing the entire scope of care, which is delivered in the household – including case management and nursing coordination – future guidelines can better support the results of the patients, the sustainability of the system and the justice of the healthcare system.”
The prescribed reimbursement for all activities for coordinating essential and adequate funds for complex cases, including adults and people with profound needs, is necessary, according to Star, the accessibility of the behavioral authority in home behavior medicine is necessary.
The wish list of stars of regulatory changes that support access to integrated, behavior -related health care at home includes permanent access to telemedicine, the elimination of arbitrary limits such as the number of years of service that have been approved, and the complete financing of the necessary services for patients with complex needs that may need several employees for a single customer.
It is also necessary to fix age gaps in reporting, said Star. Medicaid often no longer hears at the age of 21, and Medicare generally does not cover ABA services at all and does not let patients who could benefit these services without care.
Star said for services that are carried out behind the scenes, said Star.
“At the moment, our clinicians spend a lot of time to coordinate the care with other providers (such as speech therapists, occupational therapists and doctors of basic care), but the services are not reimbursable,” said Star. “This makes it difficult to really integrate the supply and build a strong team around the patient. We need unbound codes so that they can be compensated for all the important work they do if they are not directly face -viewed with the customers.”
According to Palumbo, value -oriented agreements can help to improve access to behavior medicine in behavior. According to Star, however, the standardization of the results for behavioral conditions is difficult because the goals of every person are unique.
“You want to ensure that value -oriented care does not increase the risk that people will be institutionalized,” said Heaaphy. “What is really important is that the fee for the service system is broken because there is no responsibility for the results.”
